A proper diet is critical for dialysis patients to manage chronic kidney disease (CKD) effectively. It helps balance nutrients‚ reduce symptoms‚ and slow disease progression. A well-planned diet‚ tailored to individual needs‚ can significantly improve treatment outcomes and overall quality of life. This article explores the essential dietary guidelines‚ key nutrients to monitor‚ and practical tips for maintaining a healthy diet while on dialysis. Understanding these principles can empower patients to take control of their health with the support of healthcare providers and dietitians.
Overview of the Importance of Diet for Dialysis Patients
Diet plays a pivotal role in managing chronic kidney disease (CKD) and improving outcomes for dialysis patients. A well-balanced diet helps regulate electrolytes‚ fluids‚ and waste products‚ reducing the strain on the kidneys. By limiting harmful substances like excess phosphorus‚ potassium‚ and sodium‚ patients can prevent complications such as bone disease and fluid overload. Additionally‚ proper nutrition supports overall health‚ maintaining energy levels and preventing malnutrition. A tailored diet‚ created with the guidance of a dietitian‚ is essential for managing CKD progression and enhancing the effectiveness of dialysis treatment. It empowers patients to take control of their health and improve their quality of life.
Objective of the Article
This article aims to provide a comprehensive guide for dialysis patients on managing their diet effectively. It seeks to educate patients on the importance of nutrition in maintaining kidney health and overall well-being. The article will cover essential dietary recommendations‚ including protein‚ sodium‚ potassium‚ and phosphorus intake‚ as well as fluid management. It will also discuss the role of electrolytes‚ minerals‚ and supplements in maintaining balance. Additionally‚ the article will offer practical tips for meal planning‚ tracking‚ and adjusting diets based on individual needs. The goal is to empower patients with the knowledge and tools necessary to adhere to their dietary plans and improve their quality of life while on dialysis.
Understanding Dialysis and Chronic Kidney Disease (CKD)
Dialysis is a treatment for kidney failure‚ performing functions kidneys can no longer do‚ like filtering waste and excess fluids; Chronic Kidney Disease (CKD) progresses through stages‚ with dialysis becoming necessary in advanced cases. Understanding how dialysis works and its role in managing CKD is essential for patients to make informed decisions about their care and lifestyle adjustments‚ including dietary changes that support their treatment and overall health.
What is Dialysis and How Does It Work?
Dialysis is a medical treatment that filters waste products‚ excess fluids‚ and electrolytes from the blood when the kidneys are no longer able to perform these functions. It is typically required for patients with end-stage renal disease (ESRD) or acute kidney failure. There are two main types of dialysis: hemodialysis‚ which uses a machine to cleanse the blood outside the body‚ and peritoneal dialysis‚ which uses the lining of the abdomen as a filter. Dialysis helps maintain bodily functions‚ preventing complications like fluid overload and electrolyte imbalances. A proper diet plays a crucial role in supporting dialysis effectiveness and overall patient health‚ ensuring optimal nutrient balance and reducing strain on the treatment process. Regular dialysis sessions‚ combined with dietary adjustments‚ help patients manage their condition and improve quality of life. Understanding how dialysis works is essential for making informed decisions about treatment and lifestyle changes. By adhering to a tailored diet‚ patients can better manage their health and maintain stability during dialysis. This balance is vital for preventing complications and ensuring the treatment’s success. A well-managed diet not only supports dialysis but also helps maintain overall well-being‚ reducing the risk of related health issues such as anemia or bone disease. Thus‚ dialysis and diet are closely interconnected‚ both critical components of managing chronic kidney disease effectively. This holistic approach ensures patients receive comprehensive care‚ addressing both their physical and nutritional needs. By understanding dialysis and its relationship with diet‚ patients can take an active role in their healthcare‚ leading to better outcomes and improved quality of life. This integrated care model emphasizes the importance of both medical treatment and dietary management in achieving optimal health for dialysis patients. Through education and personalized plans‚ patients can navigate the challenges of dialysis with confidence and resilience‚ ensuring their nutritional needs are met while undergoing treatment. This collaborative effort between healthcare providers and patients is key to successful dialysis outcomes and overall well-being. By prioritizing both dialysis and diet‚ patients can effectively manage their condition and enjoy a more stable‚ healthier life despite chronic kidney disease. This comprehensive approach highlights the vital role of dialysis and diet in maintaining patient health and preventing further complications. By understanding and adhering to these principles‚ patients can take control of their health journey‚ making informed decisions that support their treatment and enhance their quality of life. This synergistic relationship between dialysis and diet underscores the importance of a holistic care plan tailored to individual needs. Through continuous monitoring and adjustments‚ patients can optimize their treatment outcomes and thrive despite the challenges of chronic kidney disease. This focus on both medical and nutritional care ensures that patients receive the support they need to manage their condition effectively‚ leading to better health and well-being. By embracing this integrated approach‚ patients can face the future with confidence‚ knowing they are taking proactive steps to manage their health. This commitment to comprehensive care is essential for achieving the best possible outcomes in dialysis patients‚ emphasizing the inseparable link between treatment and nutrition. Through education‚ collaboration‚ and personalized care‚ patients can navigate the complexities of dialysis and diet‚ ensuring a brighter‚ healthier future. This dedication to holistic health management empowers patients to take charge of their well-being‚ fostering resilience and hope in the face of chronic kidney disease. By understanding the interconnectedness of dialysis and diet‚ patients can make informed choices that enhance their treatment and improve their quality of life. This knowledge and proactive approach are vital for achieving optimal health outcomes and maintaining independence. Through continuous learning and adaptation‚ patients can master the challenges of dialysis and diet‚ ensuring they receive the care they need to thrive. This journey of education and empowerment is central to successful dialysis management‚ highlighting the importance of both medical treatment and nutritional balance. By prioritizing these aspects‚ patients can achieve stability‚ reduce complications‚ and enjoy a fulfilling life despite their condition. This comprehensive strategy underscores the critical role of dialysis and diet in managing chronic kidney disease‚ offering patients a pathway to better health and well-being. Through dedication and the right support‚ patients can overcome the hurdles of dialysis and diet‚ emerging stronger and more resilient. This holistic approach to care is essential for maximizing treatment success and improving patient outcomes‚ demonstrating the profound impact of combining medical and nutritional interventions. By embracing this integrated model‚ patients can achieve a higher quality of life‚ navigating the challenges of dialysis with confidence and hope. This commitment to comprehensive care is vital for helping patients thrive‚ emphasizing the importance of both dialysis and diet in their health journey. Through education‚ collaboration‚ and personalized plans‚ patients can master the intricacies of their treatment‚ ensuring they receive the best possible care. This focus on holistic health management empowers patients to take control of their well-being‚ fostering a positive outlook and improved quality of life. By understanding and addressing both medical and nutritional needs‚ patients can achieve optimal dialysis outcomes‚ leading to a more stable and fulfilling life. This integrated approach to care is essential for helping patients manage chronic kidney disease effectively‚ highlighting the inseparable link between dialysis and diet. Through continuous support and education‚ patients can navigate their health journey with confidence‚ making informed decisions that enhance their treatment and overall well-being. This dedication to comprehensive care is critical for achieving the best possible outcomes in dialysis patients‚ emphasizing the importance of both medical and nutritional interventions. By prioritizing these aspects‚ patients can enjoy a better quality of life‚ reducing complications and thriving despite their condition. This holistic strategy underscores the vital role of dialysis and diet in managing chronic kidney disease‚ offering patients a pathway to improved health and resilience. Through education‚ collaboration‚ and personalized care‚ patients can overcome the challenges of dialysis and diet‚ achieving a brighter‚ healthier future. This integrated approach to health management is essential for maximizing treatment success and enhancing patient outcomes‚ demonstrating the profound impact of combining medical and nutritional care. By embracing this comprehensive model‚ patients can take control of their health‚ navigating the complexities of dialysis and diet with confidence and hope. This commitment to holistic care is vital for helping patients thrive‚ emphasizing the importance of both dialysis and diet in their journey toward better health. Through continuous learning and adaptation‚ patients can master the challenges of their treatment‚ ensuring they receive the best possible care. This focus on education and empowerment is central to successful dialysis management‚ highlighting the critical role of both medical and nutritional interventions. By understanding and addressing these aspects‚ patients can achieve optimal health outcomes‚ leading to a more stable and fulfilling life. This integrated approach to care is essential for helping patients manage chronic kidney disease effectively‚ emphasizing the inseparable link between dialysis and diet. Through dedication and the right support‚ patients can overcome the hurdles of their condition‚ emerging stronger and more resilient. This holistic strategy underscores the importance of combining medical treatment with nutritional balance‚ offering patients a pathway to improved health and well-being. By prioritizing these aspects‚ patients can enjoy a better quality of life‚ reducing complications and thriving despite their condition. This comprehensive approach to care is critical for achieving the best possible outcomes in dialysis patients‚ demonstrating the profound impact of both dialysis and diet on overall health. Through continuous support and education‚ patients can navigate their health journey with confidence‚ making informed decisions that enhance their treatment and well-being. This commitment to comprehensive care is vital for helping patients achieve optimal dialysis outcomes‚ leading to a more stable and fulfilling life. By embracing this integrated model‚ patients can take control of their health‚ mastering the challenges of dialysis and diet with resilience and hope. This holistic approach to health management is essential for maximizing treatment success and improving patient outcomes‚ emphasizing the importance of both medical and nutritional interventions. Through education‚ collaboration‚ and personalized plans‚ patients can thrive‚ achieving a brighter‚ healthier future despite chronic kidney disease. This journey of learning and adaptation is central to successful dialysis management‚ highlighting the critical role of both treatment and nutrition in achieving optimal health. By understanding and addressing these aspects‚ patients can overcome the challenges of their condition‚ enjoying a better quality of life and reducing the risk of complications. This integrated approach to care is vital for helping patients manage their health effectively‚ emphasizing the inseparable link between dialysis and diet. Through dedication and the right support‚ patients can achieve their health goals‚ leading to a more stable and fulfilling life. This holistic strategy underscores the importance of combining medical treatment with nutritional balance‚ offering patients a pathway to improved well-being and resilience. By prioritizing these aspects‚ patients can navigate their health journey with confidence‚ making informed decisions that enhance their treatment and overall quality of life. This comprehensive approach to care is essential for achieving the best possible outcomes in dialysis patients‚ demonstrating the profound impact of both
Stages of Chronic Kidney Disease (CKD)
Chronic Kidney Disease (CKD) is categorized into five stages based on the glomerular filtration rate (eGFR)‚ which measures kidney function. Stage 1 indicates normal eGFR with kidney damage‚ while Stage 5 signifies severe kidney failure‚ often requiring dialysis or a transplant. Each stage reflects declining kidney function‚ with eGFR decreasing progressively. Early stages focus on managing symptoms and slowing disease progression through lifestyle changes‚ including diet. Monitoring eGFR and adjusting treatment plans are crucial. Understanding these stages helps patients and healthcare providers tailor interventions‚ such as dietary modifications‚ to improve outcomes and delay progression to more advanced stages. Early intervention can significantly impact quality of life and long-term health.
The Role of Diet in Managing CKD
Diet plays a central role in managing Chronic Kidney Disease (CKD)‚ helping to slow disease progression and reduce symptoms. A well-planned diet can minimize strain on the kidneys by controlling protein‚ sodium‚ potassium‚ phosphorus‚ and fluid intake. As CKD advances‚ dietary adjustments become more critical to maintain nutrient balance and prevent complications. Monitoring these levels through regular blood tests ensures dietary plans remain effective. Patients in earlier stages may require less restrictive diets‚ while those nearing dialysis need stricter adherence. Collaborating with a dietitian allows for personalized adjustments‚ ensuring the diet aligns with the patient’s specific needs and health goals. A tailored approach maximizes kidney function and overall well-being.
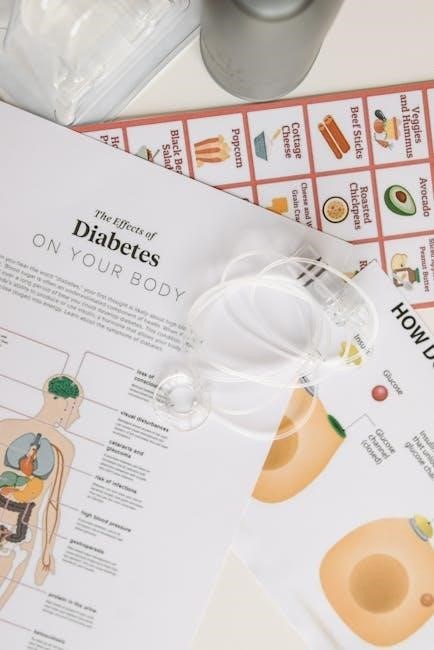
Key Dietary Considerations for Dialysis Patients
Dialysis patients must manage protein‚ sodium‚ potassium‚ phosphorus‚ and fluid intake to maintain health. A balanced diet helps reduce complications and supports treatment effectiveness.
Protein Intake: What to Consume and Avoid
Dialysis patients should focus on high-quality protein sources like lean meats‚ fish‚ eggs‚ and dairy. Plant-based options such as legumes and tofu are also beneficial. However‚ excessive protein can strain kidneys‚ so moderation is key. Avoid processed meats and high-sodium protein sources. Protein needs vary based on individual health and dialysis type. Consulting a dietitian helps tailor intake to specific requirements‚ ensuring proper nutrition without overburdening the body. Balancing protein intake supports overall health and aids in maintaining muscle mass‚ crucial for those undergoing dialysis.
Sodium Intake: Reducing Fluid Retention
Managing sodium intake is crucial for dialysis patients to minimize fluid retention and blood pressure issues. Limit sodium to 2-3 grams daily by avoiding processed foods‚ canned goods‚ and salty condiments. Opt for fresh vegetables‚ fruits‚ and low-sodium alternatives. Season meals with herbs and spices instead of salt. Monitoring sodium intake helps prevent excessive fluid buildup‚ which can strain the heart and lead to complications. Patients should also avoid adding salt during cooking or at the table. Adhering to these guidelines supports better fluid balance and overall health‚ making dialysis more effective and reducing the risk of related health problems.
Potassium Intake: Managing Levels Through Diet
Controlling potassium intake is essential for dialysis patients‚ as high levels can lead to serious heart issues. Potassium-rich foods like bananas‚ oranges‚ potatoes‚ and spinach should be consumed in moderation. Patients on peritoneal dialysis may need higher potassium intake‚ while those on hemodialysis often require stricter limits. Monitoring potassium levels through regular blood tests ensures dietary adjustments are made appropriately. Incorporating low-potassium alternatives and cooking methods‚ such as boiling vegetables‚ can help manage intake effectively. Balancing potassium consumption supports heart health and prevents complications‚ making it a critical aspect of a dialysis-friendly diet.
Phosphorus Intake: Limiting Dairy and Processed Foods
Managing phosphorus intake is crucial for dialysis patients‚ as excessive levels can harm bones and blood vessels. Dairy products‚ processed foods‚ and certain meats are high in phosphorus‚ so they should be limited. Patients are often advised to avoid foods like cheese‚ milk‚ and processed snacks. Reading food labels to identify hidden phosphorus additives is important. Incorporating low-phosphorus alternatives‚ such as non-dairy milk‚ can help maintain a balanced diet. Regular blood tests monitor phosphorus levels‚ ensuring dietary adjustments are effective. Controlling phosphorus intake supports overall health and prevents complications‚ making it a key component of a dialysis-friendly diet.
Fluid Management: Understanding Daily Limits
Fluid management is essential for dialysis patients to prevent complications like fluid overload. Typically‚ patients are advised to limit daily fluid intake to 1-1.5 liters‚ including fluids from food and drinks. Excessive fluid can lead to swelling‚ high blood pressure‚ and heart strain. Tracking fluid intake through a daily log helps ensure adherence to limits. Avoiding high-sodium foods can reduce thirst and make managing fluids easier. Patients should also be mindful of fluid-rich foods like fruits and soups. Strict adherence to fluid limits is critical to maintain health and avoid dialysis-related complications‚ ensuring the treatment remains effective and safe.
Managing Electrolytes and Minerals
Electrolytes like potassium‚ phosphorus‚ and calcium must be carefully managed to prevent imbalances. Monitoring levels through diet and supplements helps maintain overall health and prevent complications.
Calcium and Vitamin D: Balancing for Bone Health
Calcium and vitamin D are crucial for maintaining strong bones in dialysis patients. Chronic kidney disease disrupts the body’s ability to activate vitamin D‚ leading to calcium imbalances. Low calcium levels can cause bone diseases like osteoporosis or osteodystrophy. Dialysis patients often require calcium supplements and vitamin D analogs to manage these deficiencies. Dietary sources of calcium‚ such as dairy products‚ may be limited due to phosphorus content‚ so alternative fortified foods or supplements are recommended. Proper balance is essential to prevent overloading‚ which can harm the heart and blood vessels. Regular monitoring and adjustments‚ guided by a dietitian‚ ensure optimal bone health and overall well-being.
Iron and Anemia: Dietary Sources and Supplements
Iron deficiency is common in dialysis patients‚ often leading to anemia. Increasing dietary iron intake can help manage this condition. Foods rich in iron include red meat‚ poultry‚ fish‚ beans‚ lentils‚ spinach‚ and fortified cereals. Pairing iron-rich foods with vitamin C sources enhances absorption. However‚ dietary iron alone may not be sufficient‚ so supplements or intravenous iron may be necessary. Regular blood tests monitor iron levels and hemoglobin to ensure proper treatment. Balancing iron intake with medical guidance is essential to avoid overload and maintain overall health. Adequate iron management supports energy levels and improves quality of life for dialysis patients.
Other Minerals: Magnesium and Zinc
Magnesium and zinc are essential minerals for dialysis patients‚ supporting immune function‚ nerve health‚ and energy production. Dialysis can disrupt their balance‚ requiring careful management. Magnesium-rich foods include dark leafy greens‚ nuts‚ and whole grains‚ while zinc is found in meats‚ shellfish‚ and fortified cereals. However‚ high-phosphorus foods often contain magnesium‚ so moderation is key. Zinc absorption is improved with animal-based sources. Supplements may be necessary but should be taken cautiously to avoid overload. Regular blood tests help monitor levels‚ ensuring optimal health and preventing complications. Balancing these minerals supports overall well-being and complements dialysis treatment effectively‚ enhancing quality of life for patients.
Monitoring and Adjusting Your Diet
Regular blood tests track key levels like potassium‚ phosphorus‚ and sodium‚ guiding dietary adjustments. Work with a dietitian to tailor plans and maintain optimal health through personalized changes.
Regular Blood Tests and Their Significance
Regular blood tests are essential for monitoring nutrient levels‚ such as potassium‚ phosphorus‚ and sodium‚ in dialysis patients. These tests help assess how well the diet is working and identify potential imbalances. Elevated potassium levels can lead to heart complications‚ while high phosphorus levels may weaken bones. Sodium levels indicate fluid balance‚ which is critical for dialysis efficiency. Blood tests also track waste products‚ like urea‚ to ensure dialysis is effectively removing toxins. Based on these results‚ dietitians can adjust meal plans to optimize health outcomes. Regular testing ensures patients stay within safe ranges‚ preventing complications and supporting overall well-being through tailored dietary adjustments.
Working with a Dietitian for Personalized Plans
Collaborating with a dietitian is crucial for dialysis patients to develop a personalized nutrition plan. A dietitian assesses individual needs‚ medical history‚ and lab results to create tailored dietary recommendations. They help manage protein‚ sodium‚ potassium‚ and phosphorus intake while ensuring adequate nutrition. Regular follow-ups allow adjustments based on health changes or test results. A dietitian also educates patients on food choices‚ portion control‚ and meal preparation‚ empowering them to make informed decisions. This partnership is key to maintaining optimal health‚ preventing complications‚ and enhancing the effectiveness of dialysis treatment. A well-designed plan not only supports physical well-being but also improves overall quality of life.
Keeping a Food Diary for Better Tracking
Keeping a food diary is an effective way for dialysis patients to monitor their dietary intake and ensure adherence to nutritional guidelines. By recording daily food consumption‚ patients can track protein‚ sodium‚ potassium‚ and phosphorus intake‚ helping to manage these levels effectively. A food diary also aids in identifying patterns and potential areas for improvement. It provides valuable information for healthcare providers‚ enabling them to offer personalized advice and adjustments to the diet plan. Consistently maintaining a food diary fosters accountability and helps patients make informed decisions‚ ultimately supporting better health outcomes and improved management of chronic kidney disease.

The Role of a Dietitian and Caregivers
A dietitian and caregivers play a crucial role in helping dialysis patients manage their diet‚ providing personalized guidance‚ emotional support‚ and practical assistance to ensure adherence to dietary recommendations.
How a Dietitian Can Help Manage Your Diet
A dietitian specializes in creating personalized meal plans tailored to the needs of dialysis patients. They assess nutritional requirements‚ monitor lab results‚ and adjust diets to maintain optimal health. Dietitians educate patients on food choices‚ portion control‚ and nutrient balance‚ ensuring adherence to restrictions on sodium‚ potassium‚ phosphorus‚ and fluids. They also address challenges like protein intake and electrolyte imbalances‚ offering practical solutions. Regular follow-ups allow dietitians to track progress and make necessary adjustments. Their expertise empowers patients to make informed decisions‚ improving overall well-being and ensuring the best possible outcomes during dialysis treatment. A dietitian’s guidance is invaluable for managing the complexities of a dialysis-friendly diet.
Support from Family and Caregivers
Family and caregivers play a crucial role in helping dialysis patients adhere to their diet. Emotional support and encouragement can significantly improve adherence to dietary restrictions. Caregivers can assist with meal planning‚ grocery shopping‚ and food preparation‚ ensuring meals are nutritious and align with dietary guidelines. Education for caregivers about the importance of diet in managing CKD can empower them to provide better support. Open communication between patients and caregivers fosters a collaborative approach to maintaining health. A supportive environment can reduce stress and make dietary adjustments more manageable‚ ultimately improving the patient’s overall well-being and treatment outcomes.

Meal Planning and Recipes
A well-structured meal plan is essential for dialysis patients‚ focusing on balanced nutrients while adhering to dietary restrictions. Incorporating low-sodium‚ low-phosphorus‚ and potassium-friendly ingredients ensures meals are both nutritious and flavorful. Creative recipes can help patients enjoy their meals without compromising their health. Practical cooking tips‚ such as seasoning without salt and using herbs for flavor‚ can make meal preparation easier and more enjoyable. Tailored meal plans‚ with clear guidelines‚ empower patients to maintain a healthy diet while managing their condition effectively.
Healthy Cooking Tips for Dialysis Patients
Cooking for dialysis patients requires careful attention to nutrient balance and flavor. Use herbs and spices instead of salt to season meals‚ reducing sodium intake. Opt for baking‚ grilling‚ or steaming to avoid adding extra fats. Limit phosphorus by using phosphate-free substitutes in recipes. Incorporate potassium-friendly vegetables like cabbage and carrots. Avoid processed foods high in sodium and phosphorus. Use fresh ingredients to ensure optimal nutrient control. Consider portion sizes to maintain dietary restrictions. Experiment with low-sodium broth for soups and stews. Pair meals with dialysis-friendly sides like rice or quinoa. These tips help create delicious‚ nutritious meals that support overall health and well-being.
Sample Meal Plans and Recipes
Creating balanced meal plans for dialysis patients involves focusing on low-sodium‚ potassium‚ and phosphorus options. A typical breakfast might include scrambled eggs with spinach‚ whole-grain toast‚ and a small apple. Lunch could feature grilled chicken‚ roasted vegetables like carrots and green beans‚ and a side of brown rice. Dinner might include baked cod‚ quinoa‚ and steamed zucchini. Snacks like fresh berries or unsalted almonds are also dialysis-friendly. Recipes often use herbs and spices for flavor instead of salt. Consulting a dietitian ensures meals are tailored to individual needs‚ promoting better health outcomes and adherence to dietary restrictions while keeping meals enjoyable and varied.

Emotional and Psychological Aspects
Dietary restrictions for dialysis patients can lead to emotional challenges‚ including frustration and anxiety. Mental health support and a strong support system are crucial for coping effectively and maintaining well-being.
Coping with Dietary Restrictions
Dietary restrictions for dialysis patients can lead to emotional challenges‚ including frustration and anxiety. It is important to acknowledge these feelings and seek support. Gradual adaptation to dietary changes can make the process more manageable. Meal planning and exploring new recipes can help maintain variety and satisfaction. A dietitian can provide personalized guidance‚ making the transition easier. Additionally‚ involving family and caregivers in meal preparation fosters a sense of community and reduces feelings of isolation. Keeping a food diary can also help track progress and identify patterns. Remember‚ adherence to dietary guidelines is crucial for health‚ but it doesn’t have to feel overwhelming with the right strategies and support.
Mental Health and the Importance of Support
Dialysis patients often face emotional and psychological challenges‚ including stress‚ anxiety‚ and depression. These feelings can stem from dietary restrictions‚ lifestyle changes‚ and the burden of chronic illness. Support from family‚ friends‚ and healthcare providers is crucial to maintaining mental well-being. A strong support system can help reduce feelings of isolation and frustration. Open communication about emotional struggles is essential‚ as it allows for tailored interventions and encouragement. Mental health should be prioritized alongside physical health‚ as it significantly impacts overall quality of life and treatment success. With the right support‚ patients can better cope with their condition and maintain a positive outlook.

Resources and Support
Diet guides‚ cookbooks‚ and online forums provide valuable resources. Professional organizations like NKF offer support. Connecting with others through communities or hotlines can ease challenges and share experiences.
Recommended Books and Guides
Several books and guides provide comprehensive insights into dialysis diets. Titles like The Renal Diet Plan and Kidney-Friendly Cooking offer practical meal ideas and nutrition advice. The National Kidney Foundation (NKF) publishes detailed guides on managing CKD through diet. Additionally‚ The Kidney Disease Solution by Dr. Duncan Capicchiano is a popular resource for understanding dietary management. These materials are designed to help patients and caregivers navigate the complexities of kidney-friendly eating‚ ensuring they make informed choices for better health outcomes. Consulting these resources can complement professional guidance and empower individuals to maintain a balanced diet tailored to their needs.
Online Communities and Forums
Online communities and forums provide valuable support and resources for dialysis patients. Platforms like Facebook groups‚ Reddit forums‚ and specialized health websites offer spaces to share experiences and advice. Many patients benefit from communities focused on kidney health‚ where they can discuss dietary challenges and exchange recipes. The National Kidney Foundation and Kidney.org host forums where patients can connect with others and access expert guidance. These online spaces foster a sense of belonging and provide practical tips for managing dietary restrictions. Engaging with these communities can help patients feel supported and informed as they navigate their treatment journey.
Encouragement for Adherence and Hope
A well-managed diet is crucial for dialysis patients‚ helping to manage symptoms‚ slow disease progression‚ and improve treatment outcomes. Adherence to dietary guidelines can significantly enhance quality of life.
